Veterans and Cannabis

The weekend after 4/20 I attended the National Cannabis Festival in Washington DC and spent most of my time in the Veterans Wellness Lounge. I interacted with vets of all ages, genders,
and backgrounds, and discussed the impact of their service experience on their physical and emotional health, and the impact that medical cannabis has had on their symptoms.
In the film Unprescribed (a film by veteran Steve Ellmore now screening on Amazon Prime) veteran Boone Cutler mentions that because of advances in medical science, soldiers returning
from war now survive far more grievous physical and psychological injuries than ever before – but upon their arrival home, “No one knew how to treat us, so they gave us pills. Lots and lots of
pills.” These regimens, which often include many different pain medications (opiates, muscle relaxants, NSAIDs) and a variety of psychotropic medications (antidepressants, anxiolytics,
antipsychotics, mood stabilizers, stimulants) are known as “combat cocktails” or “zombie dope.” They alter and impair their mental status to the point where some veterans eventually believe
that suicide is the best option. Currently, we are losing 22 veterans/day to suicide, twice as many as those who have never served. However, many veterans are now successfully turning
to medical cannabis for relief from their despair and hopelessness.
There have been accounts of soldiers experiencing psychological symptoms after military trauma from as far back as ancient times. 70% of all adults report experiencing Post-Traumatic Stress Disorder (PTSD) at least once in their lifetime, and it affects ~8 million Americans per year. 12-20% of veterans who served in Iraq and Afghanistan have been diagnosed with PTSD, among Gulf War veterans the rate is 12-31%, and with Vietnam veterans the rate has been 30% and higher. Higher rates are seen among soldiers who experienced Military Sexual Trauma (MST), and with combat veterans who experience physical injuries and TBIs (traumatic brain injuries).
PTSD is often under-diagnosed because veterans feel ashamed of their symptoms, and among soldiers who are diagnosed, 74% develop co-morbid substance dependence. In the general population, males have a suicide rate of 19.4 per 100,000 compared to females with a rate of 4.9 per 100,000, but among veterans who are VA users the rate is 38.3 per 100,000 for males and 12.8 per 100,000 for females. PTSD from combat trauma increases the risk.
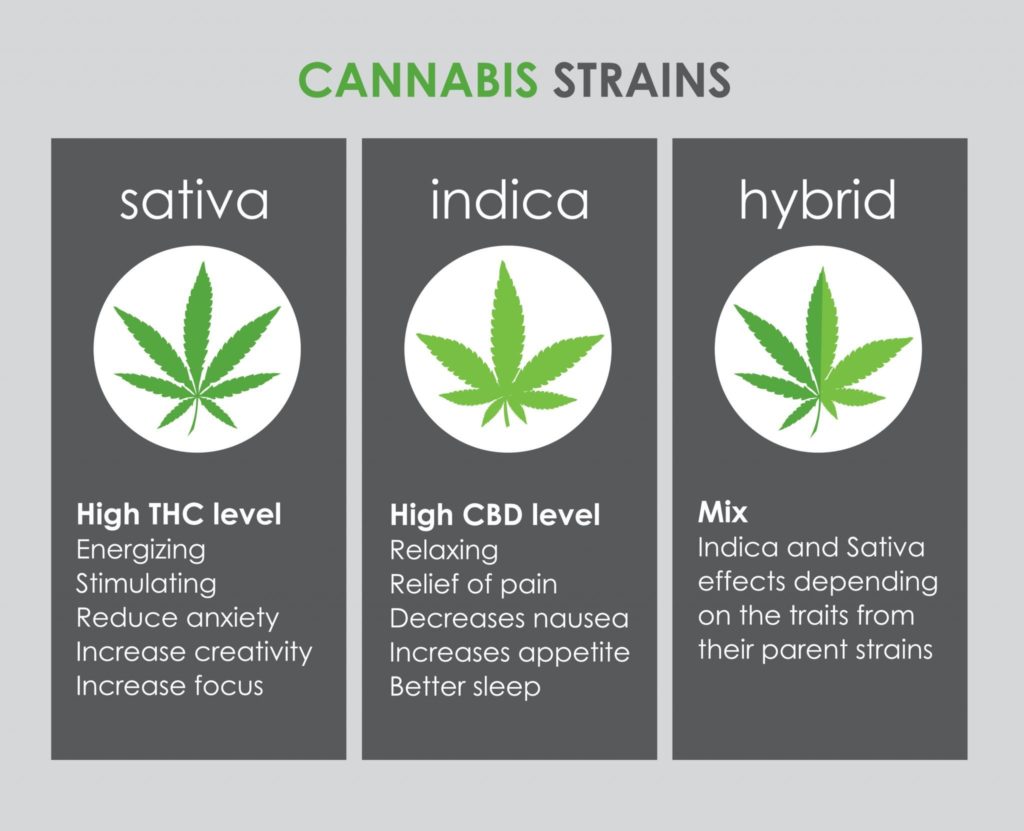
Medical cannabis could serve an important role in decreasing the symptoms veterans experience when dealing with their physical and psychological traumas. It may have impact on a wide range of physical and psychological conditions without “polypharmacy” – the combination of many different medications without a clear understanding of their interactions. In offering relief from pain, inflammation, insomnia, GI upset, anxiety, PTSD, autoimmune disorders, and several other conditions, cannabis can serve to greatly improve a patient’s quality of life.
Additionally, the social impact, and the way cannabis aids patients in feeling less isolated and better able to enjoy social interactions, shows why cannabis is so effective. It assists veterans
and non-veterans alike in surviving and flourishing after psychological and physical traumas. Add to this the remarkably benign safety profile cannabis has, with no lethal dose and no
serious toxicities, cannabis is an excellent place to begin treatment for both the physical and emotional issues our veterans face.